Revitalizing Health: Texas Leads with MAHA Legislation Amid Exposures of Systemic Health Challenges
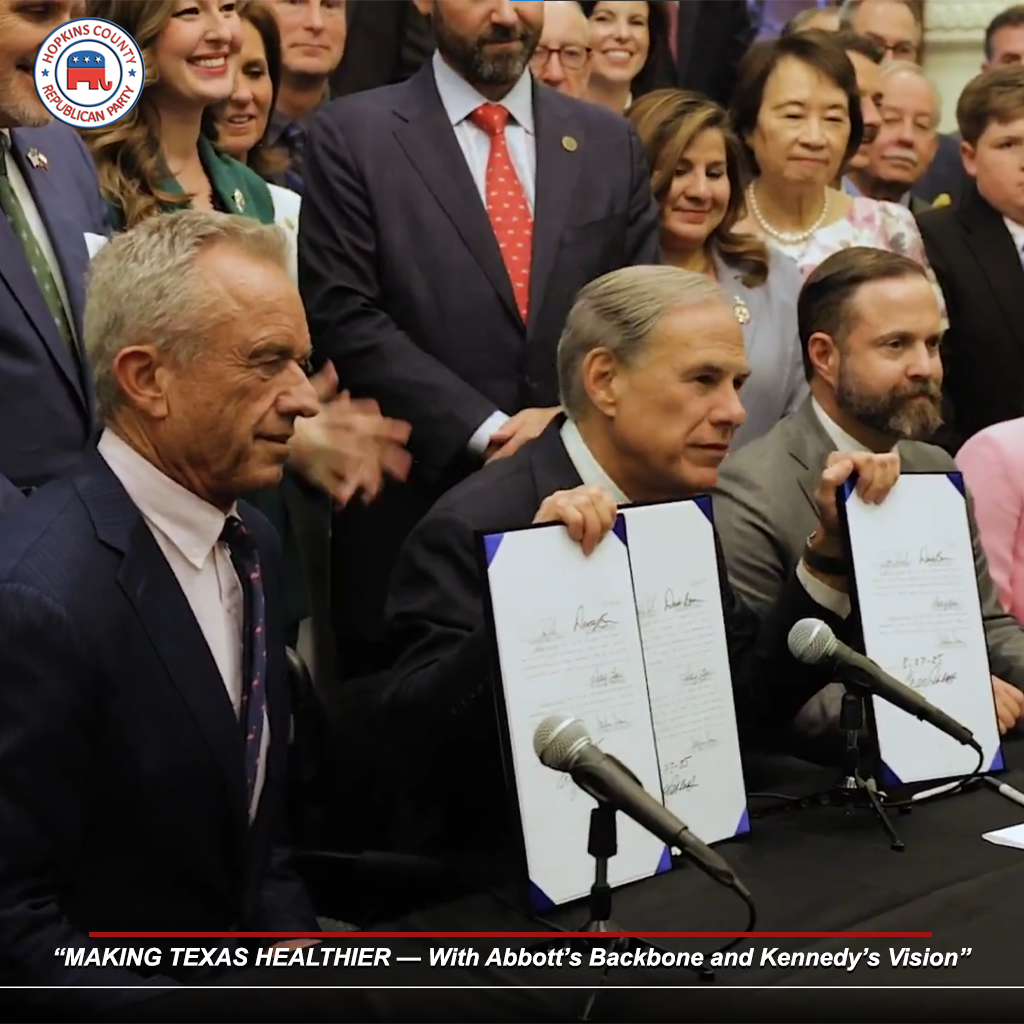
On August 27, 2025, Texas Governor Greg Abbott signed key legislation inspired by the Make America Healthy Again (MAHA) initiative, aimed at promoting healthier living across the state. The ceremonial signing, attended by U.S. Secretary of Health and Human Services Robert F. Kennedy Jr., included Senate Bill 25, known as the “Make Texas Healthy Again” Act, which embeds nutrition education in schools and prohibits the use of federal food assistance for sodas and candy. Additional bills, Senate Bill 314 and Senate Bill 379, were also enacted to support rural healthcare and ban certain food additives in school meals. Following the signing, Abbott and Kennedy met with rural healthcare leaders to discuss initiatives, including a $50 billion federal allocation for rural healthcare, with Texas receiving $100 million annually for five years. Abbott stated that Texas, in collaboration with the Trump Administration, will lead the nation in improving healthcare outcomes.
Kennedy, as HHS Secretary, has focused on addressing corruption within the Food and Drug Administration (FDA) and food corporations. He has highlighted how food companies incorporate unhealthy ingredients, such as artificial dyes and additives, contributing to chronic health issues that benefit the healthcare system financially. Kennedy’s efforts include a $500 million initiative to pressure companies to remove such additives, linking them to population-wide health declines and increased profits for pharmaceutical and medical sectors. This aligns with broader critiques of the FDA’s role in allowing contaminated foods and ineffective medical products, which Kennedy describes as part of a corrupt system prioritizing industry over public health.
Processed foods contain hundreds of chemical additives, including artificial food colorings, which have been associated with various health effects. Studies indicate that synthetic food dyes may contribute to behavioral issues in children, such as hyperactivity, and broader risks including obesity, metabolic syndrome, cardiovascular diseases, and cancers. Artificial colors like Red Dye #3 have been linked to cancer, particularly thyroid tumors, and neurobehavioral problems like ADHD. Other additives, including preservatives and flavor enhancers, have been identified as endocrine disruptors, potentially affecting hormone function, immune systems, thyroid health, and fertility. In 2025, the FDA announced plans to phase out petroleum-based synthetic dyes, substituting them with natural ingredients, following evidence of harm to memory, learning, and behavior in children.
Historically, heart disease prevalence in the United States was low before the 1900s, with heart attacks considered rare events prior to that period. Data indicate that coronary heart disease rates began rising significantly from 1900 through the late 1960s, attributed to increases in coronary atherosclerosis. Concurrently, healthcare spending on cardiovascular conditions escalated, from $212 billion in 1996 to $320 billion in 2016, even as the population grew by over 52 million. Overall health expenditures in the U.S. rose from 5% of GDP in 1960 to 18% in 2016, with much of the increase linked to heart disease management. By 2015, heart disease and stroke costs reached over $320 billion annually in medical expenses and lost productivity.
The breakfast industry has promoted sugary foods as a standard morning meal, evolving from health-focused origins. The term “breakfast” derives from “breaking the fast,” referring to ending the overnight period without food, a concept traced back to Middle English in the 15th century. Cold cereals, invented in 1863 as a digestive aid, shifted toward sugary varieties post-World War II when sugar rationing ended, allowing companies to market them as energy sources. This promotion established processed, ready-to-eat options as dominant, often featuring added sugars, artificial sweeteners such as Aspartame and Sucralose, high fructose corn syrup, artificial colors, and freeze-dried fruits. Similarly, the pork industry, facing declining sales in the 1920s, orchestrated a campaign to integrate bacon into breakfast, significantly contributing to rising health issues. Edward Bernays, hired by the Beech-Nut Packing Company, surveyed 5,000 physicians to endorse bacon as part of a “hearty” breakfast, rebranding it from a seasonal or lunch item to a daily staple. This marketing push, which ignored the high saturated fat and sodium content of processed pork products, increased sales despite overall pork demand dropping 9% over the past two decades, with per capita consumption falling from 51.8 pounds in 2000 to 47.1 pounds in 2020. The campaign’s success, followed by pork belly futures contracts in 1961 to stabilize sales, prioritized industry profits over public health, contributing to a 42% higher risk of coronary heart disease per 50 grams daily intake of processed meats, according to a 2010 meta-analysis. This dietary shift fueled the cardiovascular epidemic, increasing reliance on pharmaceutical interventions like cholesterol-lowering drugs.
Cholesterol-lowering medications, such as statins, have been linked to potential brain effects, including reduced cholesterol in neural tissues, which may contribute to cognitive issues. Studies show statins are associated with higher white matter hyperintensity volumes and lower cortical gray matter, indicating impacts on brain structure. Reports of memory loss and fuzzy thinking in a small portion of users have raised concerns, with the FDA noting potential neurocognitive effects in 2012. These side effects are tied to statins’ ability to cross the blood-brain barrier, influencing brain cholesterol metabolism, which is critical for neuronal function. Fluctuating cholesterol levels in older adults have also been linked to increased dementia risk, with a 2020 study finding that cholesterol variability correlates with higher Alzheimer’s risk. Public health campaigner and cardiologist Dr. Aseem Malhotra has criticized the overemphasis on LDL cholesterol as a primary driver of heart disease, arguing that cholesterol buildup in arteries often reflects underlying inflammation or endothelial damage, with the body producing cholesterol as a protective patch to repair damaged vessels. Malhotra advocates addressing root causes like poor diet and chronic inflammation rather than relying solely on statins. A 2019 pooled analysis of 30 cohort studies found that higher dietary intake of omega-6 fatty acids, while common in processed foods, was associated with increased cardiovascular mortality when not balanced with omega-3s, highlighting the need for dietary interventions over pharmaceutical reliance. As an alternative, supplements like L-Ornithine, which converts to L-Arginine in the body, have been shown to improve endothelial function and reduce arterial plaque buildup by enhancing nitric oxide production, offering a preventive measure against cardiovascular issues. Additionally, coconut oil, rich in medium-chain triglycerides (MCTs), can cross the blood-brain barrier, providing an alternative energy source for brain cells. Studies, including a 2020 trial, have demonstrated that coconut oil supplementation improves cognitive function in Alzheimer’s patients by supporting neuronal energy metabolism, potentially countering the cognitive decline linked to cholesterol-lowering drugs.
Prevalence of attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) has risen markedly in recent decades. In 2022, 7.1 million U.S. children aged 3-17 (11.4%) had an ADHD diagnosis, up by 1 million from 2016. ASD rates among 8-year-olds increased from 1 in 150 in 2000 to 1 in 31 (3.2%) by 2022, a 70% rise from 2000 to 2018 and 4.8 times higher over 22 years. Diagnoses of both conditions have grown 175% over the past decade. In adults with autism, ADHD rates remain 10 times higher than the general population. Robert F. Kennedy Jr., a prominent voice in the MAHA movement, has controversially linked the rise in ADHD and ASD to vaccines, particularly claiming that ingredients like thimerosal, a mercury-based preservative, contribute to neurological disorders. Kennedy also argues that modern processed foods, stripped of essential vitamins and minerals due to industrial farming and processing, exacerbate these conditions by depriving developing brains of critical nutrients like zinc, iron, and vitamin D. Big Pharma and mainstream health authorities, including the CDC and FDA, assert that these claims are false or debunked, citing studies like a 2015 CDC review showing no link between vaccines and autism. However, numerous reports, including a 2005 study by Kennedy himself in Rolling Stone (later retracted under pressure), and independent analyses, such as a 2014 meta-analysis showing correlations between environmental toxins and neurodevelopmental issues, suggest otherwise, pointing to potential vaccine-related and nutritional deficiencies as factors warranting further investigation. Despite these controversies, the fetal and early life environment, influenced by maternal nutrition, remains a critical factor in neurodevelopment.
Maternal nutrition, particularly omega-3 fatty acids during pregnancy, supports child brain development. Higher maternal omega-3 polyunsaturated fatty acids (PUFAs) relate to optimal long-term brain development in children. Docosahexaenoic acid (DHA), a key omega-3, is critical during the third trimester for neurogenesis and signal transduction, with supplementation linked to improved cognitive outcomes. Increases in maternal DHA correlate with higher verbal and full-scale IQ scores in children at ages 5 and 6. Limited evidence shows omega-3 supplementation may result in favorable cognitive development, enhancing neurotransmitter function and immune support postpartum. Conversely, soy-based products, such as infant formula and dietary staples, contain phytoestrogens like genistein and daidzein, which mimic estrogen in the body. Studies suggest that high exposure to these phytoestrogens in male infants may influence brain development by altering neuroendocrine pathways, potentially leading to feminized brain wave patterns. Research indicates that early exposure to soy isoflavones can affect sexual differentiation in the brain, which may contribute to gender dysphoria or confusion as the child develops. These effects are linked to the disruption of testosterone signaling during critical developmental windows, potentially impacting long-term behavioral and identity outcomes. In adult males, high soy consumption has been associated with reduced testosterone levels and increased estrogenic activity, potentially leading to gynecomastia (“man boobs”). A 2008 case study reported gynecomastia in a man consuming 3 quarts of soy milk daily, with elevated serum estradiol levels resolving after discontinuation. A 2011 meta-analysis found that high isoflavone intake (e.g., 100–300 mg/day) can reduce testosterone by up to 10–20% in some men, particularly with prolonged exposure, though effects vary by individual metabolism and gut microbiota. This hormonal imbalance may contribute to fat accumulation in the chest, mimicking breast tissue, and other feminizing effects.
Efforts to promote alternative protein sources have raised concerns about lab-grown meat, also known as cultured meat. Potential hazards include contamination with heavy metals, microplastics, nanoplastics, and allergens from additives used to improve taste and texture. Risks also encompass nutritional deficiencies, cell line dysregulation, and the possibility of cancer cell emergence in cultures. Growth hormones in production have been associated with developmental, neurobiological, genotoxic, and carcinogenic effects. Additionally, consuming insects as meat substitutes carries health risks, including allergies, particularly for those with shellfish sensitivities, due to cross-reactivity. Parasitic infections from uncontrolled feeding habits in wild-harvested insects, as well as contamination with bacteria, viruses, fungi, mycotoxins, and heavy metals, have been documented. Allergic reactions such as urticaria, edema, dyspnea, and anaphylaxis have been reported, with edible insects linked to 4.2–19.4% of food allergies in Asian populations.
Genetically modified (GMO) foods have been associated with potential health risks, including toxicity, allergic reactions, and organ damage. Studies suggest GMO consumption may lead to hepatic, pancreatic, renal, or reproductive effects, as well as increased tumor or cancer incidence, low fertility, and decreased learning abilities. The instability of genetically engineered foods could contribute to infertility, immune problems, accelerated aging, faulty insulin regulation, and changes to major organs and the gastrointestinal system.
Microplastics in food present additional risks, with exposure linked to oxidative stress, metabolic disorders, immune responses, and changes in the intestinal microbiome. These particles can cause inflammation, DNA damage, gene activity alterations, and increased risks of cancer, infertility, poorer fetal development, respiratory disorders, and cardiovascular problems. Microplastics accumulate in organs, disrupt nutrient absorption, and contribute to dysbiosis, potentially leading to abdominal pain, bloating, and impaired fasting glucose or insulin resistance.
Xenoestrogens in food, acting as endocrine disruptors, affect brain development in babies and testosterone levels in males. Prenatal exposure can alter reproductive organs, neuroendocrine systems, and lead to neurodegeneration, inflammation, oxidative damage, and decreased testosterone. These chemicals disrupt hormonal signaling, contributing to infertility, thyroid disease, and disrupted gene expression or microbiome composition. In males, xenoestrogens lower testosterone, disregulating the hypothalamic-pituitary-gonadal axis and linking to reproductive issues.
Everyday exposures extend to coatings on register receipts, often containing bisphenol A (BPA) or bisphenol S (BPS), which act as endocrine disruptors. These chemicals, absorbed through the skin, enter the bloodstream and are linked to reproductive harm, hormonal disruption, and endocrine system damage. Initially explored in the 1930s as potential female contraceptives due to their estrogen-mimicking properties, BPA and related compounds were shelved for contraceptive use after concerns about systemic toxicity. However, industry reintroduced them in thermal paper coatings despite known risks, with studies showing BPA exposure correlates with a 20–40% reduction in fertility rates and increased miscarriage risk. The widespread use of BPA and BPS in receipts, handling up to 1 mg per contact, has been associated with declining birth rates globally, alongside fertility issues, thyroid dysfunction, and elevated cancer risks, raising concerns about intentional population control through environmental exposure.
Supporting local farmers offers a path to healthier food systems, particularly in regions like Hopkins County, Texas, known as the “Dairy Capital of Texas.” The county’s dairy industry, which began in the 1930s with the arrival of the Carnation Milk Company, remains a cornerstone of its economy, with over 165 Grade A dairy farms. Farms like Wallace Family Farm in Sulphur Springs produce sustainable, all-natural eggs, while others, such as Falster Farm on Pasture 365, raise grass-fed Red Angus and Hereford beef, emphasizing nutrient-dense, chemical-free products. Free-range chicken eggs are rich in omega-3 fatty acids, vitamin D, and antioxidants, supporting heart health, brain function, and immune response compared to conventional eggs. Grass-fed dairy and beef from local farms provide higher levels of conjugated linoleic acid (CLA) and omega-3s, linked to reduced inflammation and lower risks of heart disease and obesity. The Celebration Market, held at Celebration Plaza in downtown Sulphur Springs from May 17 to September 20, 2025, every Saturday from 6 p.m. to 10 p.m., showcases locally grown produce, free-range eggs, grass-fed meats, and homemade goods. This market, featuring entertainment, a splash pad, and activities for children, fosters community engagement and supports local vendors. Additionally, the first-ever Sulphur Springs Fall Farmers Market, running Saturdays from 8 a.m. to 1 p.m., September 27 to November 15, 2025, in the grassy area next to the Tesla Charging Stations in Downtown Sulphur Springs, offers fresh produce, handmade goods, delicious food, and local fun. This market encourages community support for neighbors while providing access to high-quality, chemical-free products in the crisp fall air. By prioritizing farmers markets like these, consumers can access nutrient-rich foods free from harmful additives, countering the health risks posed by industrial food systems and reinforcing the medical oath to “Do No Harm.”
These bills that I am signing today put Texas on that pathway. Taxpayer dollars will no longer be used to fund chronic health problems in our state. These bills were truly a bipartisan effort, and I am proud to sign them into effect.
– Governor Greg Abbott